Crohn’s disease and ulcerative colitis are two distinct but clinically similar diseases classified under the name of inflammatory bowel disease.
The causes are not yet fully understood but it is known that both Crohn’s disease and ulcerative colitis have influences of genetic and environmental factors.
The most accepted theory today is that there would be a malfunction of the immune system, probably triggered by some viral or bacterial infection that would mistakenly attack normal elements of the digestive tract like bacteria, food and cells, leading to a state of chronic inflammation of the intestines, in a process similar to autoimmune diseases.
Inflammatory bowel diseases are more common in countries of the northern hemisphere and in the population of Jewish origin. It usually appears between 15 and 40 years. Men and women are equally affected. 25% of patients with inflammatory bowel disease have at least one first-degree relative also with the disease.
It has not been possible to verify any connection of the disease with some type of diet or with emotional stress. There is also no evidence of contraceptive influence.
Curiously, smoking has a divergent influence between the two diseases, since it increases the patient’s risk of developing Crohn’s, but reduces the risk of having rectocolitis.
Some studies suggest that the use of anti-inflammatory drugs may favor the onset of inflammatory bowel diseases. On the other hand, people who have withdrawn the appendix seem to have a lower risk. However, they are still in need of further investigation.
Table of Contents
DIFFERENCES BETWEEN CROHN’S DISEASE AND ULCERATIVE COLITIS
Crohn’s disease is an inflammatory bowel disease that can affect any part of the digestive tract, from the mouth to the anus. However, 80% of the patients present lesion of the distal ileum and cecal ileum, which are respectively the final portion of the small intestine and the transition region between the small intestine and the colon.
Crohn’s disease is characterized by inflammation in all layers of the gut wall, with diffuse lesions along the digestive tract. A typical characteristic of Crohn’s is to present areas of healthy gut between inflamed areas.
The ulcerative colitis attacks only the colon and rectum, sparing the other regions of the digestive tract. In the rectocolite the lesion is usually continuous and affects only the most superficial layer of the intestinal mucosa, leading to inflammation and ulcer formation.
SYMPTOMS OF CROHN’S AND ULCERATIVE COLITIS
Although they are two different diseases, the symptoms are very similar. The most common are:
– Diarrhea
– Loss of blood in stool
– Abdominal pain.
– Fever
– Weight loss.
– Tiredness.
– Anemia
Despite the similarities in symptoms, some clinical findings are more common in Crohn’s and others in rectocolitis.
Because Crohn’s disease affects all layers of the gut wall, fistulas, obstructions and perforations of the digestive tract are more common.
Intestinal perforation causes a serious picture because it facilitates the contact of feces and their bacteria with the abdominal cavity. It usually causes with peritonitis and severe sepsis
Fistulas are communications between two organs that arise due to inflammatory processes. In Crohn’s, fistulas can attach the intestine to the vagina, bladder, other regions of the intestine itself, or even to the skin.
As already explained, Crohn’s disease can affect any part of the digestive tract. However, inflammation of the rectum is characteristic of rectocolitis, which may or may not occur in Crohn’s https://zolpidemsleep.com disease. A suggestive picture of inflammatory bowel disease with no lesion in the rectum practically seals the diagnosis of Crohn’s disease.
The presence of ulcers in the colon is typical of rectocolitis, but may also occur on Crohn’s.
Stool with blood occurs in both diseases, but is more common in ulcerative colitis.
The clinical course of the disease is usually milder in rectocolitis than in Crohn’s. However, it is important to note that in both diseases there may be aggressive cases and milder cases.
Inflammatory bowel diseases manifest themselves with periods of exacerbation (crises) interspersed with periods of little or no symptomatology. The remission period can last from weeks to months.
As with Crohn, the involvement of the ileum and the ileocecal region is very common, the condition can often be reminiscent of an appendicitis, since the appendix is ??in this site.
EXTRA-INTESTINAL MANIFESTATIONS OF CROHN’S DISEASE AND ULCERATIVE COLITIS
In addition to the symptoms caused by inflammation of the gastrointestinal tract, inflammatory bowel diseases also occur with symptoms in other systems of the body. The most described are:
– Skin lesions: Pyoderma gangrenosum and erythema nodosum.
– Eye lesions: Uveitis, irites and episclerites.
– Musculoskeletal injuries: Arthritis and ankylosing spondylitis.
Amyloidosis.
– Thrombosis and embolisms
– Sclerosing cholangitis.
INFLAMMATORY BOWEL DISEASE AND CANCER
In both Crohn’s disease and colitis, the risk of colon cancer is 2 to 5 times greater than the general population.
On average, 5% of those with inflammatory bowel disease will develop colon-rectal cancer. The risk is greater the longer the disease is and the more severe and extensive the inflammation of the colon.
Therefore, after about 8 years of diagnosis of Crohn’s or rectocolitis, annual colonoscopies are indicated for the early detection of colon tumors.
DIAGNOSIS OF CROHN’S DISEASE AND ULCERATIVE COLITIS
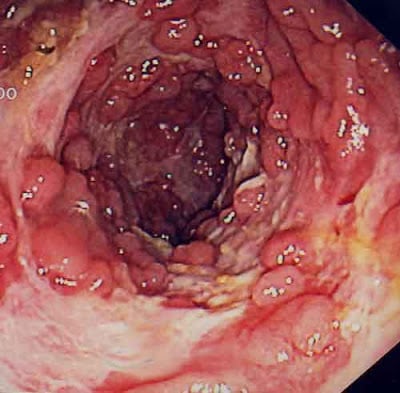
Currently the diagnosis of intestinal inflammatory diseases is performed through colonoscopy with biopsy .
The findings of ulcerations, pseudopolyps, granulomas associated with signs of inflammation of the intestinal mucosa help to establish the diagnosis, which is confirmed later with the result of the biopsies.
TREATMENT OF CROHN’S DISEASE AND ULCERATIVE COLITIS
The treatment of inflammatory bowel diseases is aimed at the control of the inflammation and consequently the improvement of the symptoms.
The two most commonly used drugs are Sulphthalazine and 5-aminosalicylate (5-ASA), also known as Asacol® and Pentasa®.
Antibiotics such as metronidazole and ciprofloxacin are also often used.
In more severe cases immunosuppressants such as corticosteroids may be used in high doses, azathioprine, 6-mercaptopurine and methotrexate.
A new class of drug, called anti-TNF has recently been incorporated into the arsenal of treatment for Crohn’s and rectocolite. The 3 drugs of this class used are Infliximab, Adalimumab and Certolizumab.
There is not yet a diet that is proven to help with inflammatory bowel diseases. What is indicated is to individually assess which foods exacerbate the symptoms to avoid them. But there is no food relationship that does badly or universally.
It is aimed at avoiding cigarette but also common anti-inflammatory drugs.
In Crohn’s disease where fistulas, perforations and obstructions are common, surgery is often necessary to remove the affected segment.
By defects in food absorption, it is common for the Crohn’s sufferer to develop some nutritional deficiencies and malnutrition. These patients often develop osteoporosis for calcium and vitamin D deficiency.